Contents of this article
What is GERD
Gastroesophageal Reflux Disease (GERD) is a chronic digestive disorder characterized by the backflow of stomach contents into the esophagus. This backflow is known as acid reflux, and it can irritate the lining of the esophagus. This occurs when the lower esophageal sphincter (LES) becomes weak or relaxes inappropriately, allowing acid and other gastric contents to rise, causing inflammation and damage to the esophageal lining with significant symptoms such as Heartburn. Acid reflux is commonly experienced now and then by many people overtime. When the acid reflux happens repeatedly over time, it can cause Gastroesophageal reflux disease (GERD).
The esophagus or gullet is a hollow tube or passage way between the throat (pharynx) and the stomach. The lower esophageal sphincter (LES) is a ring of muscle that holds the bottom of the esophagus to the opening of the stomach closed so that gastric acid does not flow back (reflux) up the esophagus. The sphincter relaxes to allow food into the stomach and close back again to prevent reflux. When this sphincter weakens, gastroesophageal reflux (GER) occurs. Repeatedly occurrence of GER over time results in GERD.
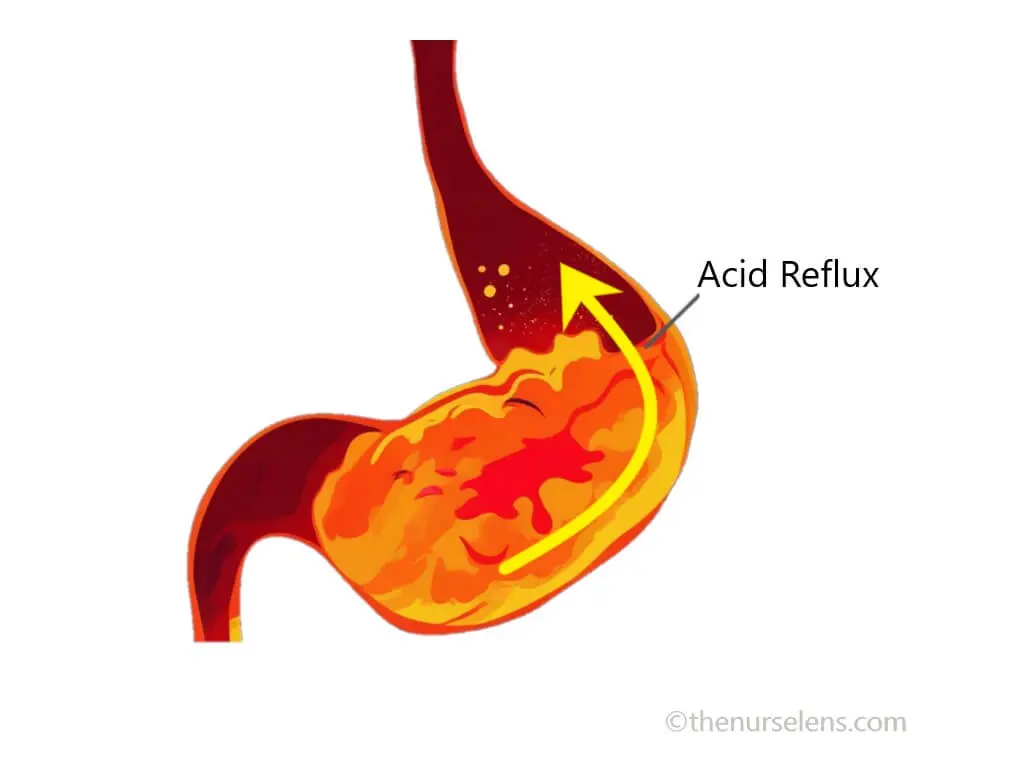
Acid Reflux
How common is GERD
GERD is a common disorder, affecting approximately 18.1% to 27.8% of adults in North America and 20% of the population in Western countries. The prevalence also varies globally, with estimates ranging from 4.16% in some regions to as high as 22.40% in others. Recent studies estimate that about half of all adults will experience reflux symptoms at some point in their lives, which indicate a significant public health concern
Risk factors of GERD
- Obesity: Excess weight, increased body mass index (BMI) can put pressure on the abdomen, weakening the LES.
- Age: Older adults are at a higher risk.
- Hiatal Hernia: This condition occurs when part of the stomach pushes through the diaphragm into the chest cavity.
- Pregnancy: Hormonal changes and increased abdominal pressure can lead to reflux.
- Connective tissue disorders, such as scleroderma.
- Smoking and alcohol intake: Tobacco use can weaken the LES and contribute to reflux.
- Diet: High intake of fatty foods and beverages, such as spicy foods, citrus, chocolate, caffeine, and alcohol, can trigger symptoms.
- Physical Inactivity: Sedentary lifestyles are associated with higher prevalence of GERD and exacerbate symptoms.
- Delayed stomach emptying can increase pressure and reflux
- Medications: Certain medications can cause heartburn and trigger GERD symptoms
Causes of GERD
The primary cause of GERD is the dysfunction of the lower esophageal sphincter (LES), the muscle that regulate the entry food into the stomach and prevents stomach contents from flowing back into the esophagus. There are several factors that may contribute to the dysfunction of the LES.
- Lifestyle factors – smoking, immediately sleeping after eating, excessive alcohol consumption, sedentary lifestyle etc.
- Health factors – connective tissue disorder, obesity, old age, etc.
- Esophageal Motility Disorders - Abnormal contractions in the esophagus can contribute to GERD symptoms.
Pathophysiology of GERD
Gastroesophageal reflux is primarily as a result of the lower esophageal sphincter (LES). Gastric outflow resistance increases intragastric pressure leading to reflux. This occurs when the LES becomes incompetent allowing the backward movement of gastric content (reflux) into the esophagus. This impairs salivary functions and esophageal peristalsis, decreasing clearance of the acid refluxed, damaging mucosal lining of the esophagus.
Signs & Symptoms of GERD
Common symptoms of GERD include
Heartburn (acid indigestion): A burning sensation in the chest, often after eating or at night causing discomfort. This discomfort occurs when stomach content flows back into the esophagus, the tube connecting the pharynx (throat) to the stomach. It can feel like a painful pressure or burning behind the breastbone, coming back to the mouth and may be accompanied by an acid or sour taste in the mouth. Heartburns can last for about hour or more
- Regurgitation: The felling or sensation of acid backing up into the throat or mouth.
- Difficulty swallowing (Dysphagia)
- Persistent chronic cough, particularly at night.
- Hoarseness or sore throat, this is due to acid irritation.
- Chest Pain
- Nausea or vomiting
- Weight loss
Diagnostic Investigations & Test
Diagnosis of GERD typically involves a clinical assessment based on the presenting symptoms and response to acid suppression therapy. Important diagnostic methods include the following:
Endoscopy:An upper endoscopy, a procedure using a flexible thin tube with a camera at the end to examine the upper digestive tract. This test can also be used to take tissue sample of the esophagus for biopsy to test for Barrett esophagus and can dilate the esophagus when narrowed during the procedure.
Esophageal pH Monitoring:Measuring acid levels in the esophagus over 24 hours. This test tracks the acidity during various activities, including meals, physical activity, and sleep. This method involves placing a small capsule in the esophagus that measures acid levels for up to 96 hours, providing comprehensive data on acid exposure over time. This method is considered the gold standard for determining acid reflux
History and Physical Examination
Transnasal esophagoscopy
Esophageal Manometry
X-ray of the upper digestive tract.
You may also like: Everything you need to know about Gastritis
Medical Management of GERD
Management strategies for GERD focus on reducing the amount of acid reflux to alleviate symptoms and prevent damaging the esophageal lining and to reduce complications. Certain lifestyle habits and home remedies may help treat symptoms. If symptoms persist for few days to weeks, certain Over-the-counter (OTC) medications and additions test may recommend by prescriber to manage GERD.
Lifestyle Modifications:Weight loss, dietary changes, avoiding certain triggers such as smoking and excessive alcohol intake, and elevating the head during sleep reduce the risk of getting GERD.
Medications options include:
Antacids:Neutralize stomach acid which help prevent heartburn. Examples of antacids include Tums, Rolaids, Sodium bicarbonate (Alka-Seltzer), Calcium carbonate (Osteo MD), Magnesium hydroxide (Mylanta), Aluminum hydroxide (Amphojel)
Histamine 2 (H2) Blockers:Block acid secretion in the stomach reduce acid production. H2 blockers include Nizatidine (Axid), Ranitidine, Famotidine (Pepcid), Cimetidine (Tagamet).
Proton Pump Inhibitors (PPIs):Also known as acid pumps, stronger acid reducers. They block the protein needed for the production of gastric acid. Example of PPIs, omeprazole (Prilosec), esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec), pantoprazole (Protonix)
In severe cases, surgery is an option for treatment of GERD for people who cannot tolerate medication. A minimally invasive Surgical intervention called fundoplication is considered to strengthen the LES.
Nursing Management of GERD
The following are the measures to put in place in the care of patient's with GERD
- Assess patient for location and intensity of pain
- Assess patient pain characteristics using a standardized scale, e.g. Pain rating scale
- Assess patient for heartburn
- Provide emotional support to reduce anxiety
- Monitor daily caloric intake
- Provide small, frequent meals at regular interval
- Serve patient diet low in fat, high in fiber
- Instruct patient to remain in upright position at least 2 hours after meals
- Encourage patient to avoid food or drink 2 hours before bedtime
- Instruct patient to avoid irritants, such as highly seasoned foods, acidic juices, alcohol, caffeine, bed time snacks and tobacco
- Teach patient about relaxation techniques to reduce stress-induced acid production
- Position patient in semi-Fowler’s position to decrease acid reflux
- Assess patient for signs of complications such as Barrett’s esophagus
- Monitor patient for signs of aspiration
- Educate patient on condition
- Educate patient on smoking cessation
- Administer medications as prescribed and monitor side effect
- Ensure patient compliance with the medication regimen
Complications of GERD
Untreated GERD can lead to several complications such as
- Esophagitis
- Esophageal Strictures
- Barrett's Esophagus
- Esophageal Cancer
Preventive measures
- Exercise regularly to maintain a healthy weight and reduce symptoms
- Reducing obesity can significantly lower the risk of GERD.
- Avoiding foods and beverages that trigger symptoms.
- Avoid food and medications and that trigger GERD symptoms or stimulate acid production
- Raising the head end of the bed
- Quit smoking
- Avoid late meal - Nightmare symptoms can be avoided by eating early in the evening
- Wait at least three hours before going to bed after eating
References
- American Gastroenterological Association. (2023). Gastroesophageal Reflux Disease (GERD).
- Epidemiology, Causes, and Management of Gastro-esophageal Reflux Disease: A Systematic Review – PMC
- Gastroesophageal Reflux Disease (GERD) - PMC
- Johnson, L. F., & DeMeester, T. R. (2023). The Role of Lifestyle Modifications in the Management of GERD. Gastroenterology Clinics of North America.
- Katz, P. O., et al. (2023). Guidelines for the Diagnosis and Management of Gastroesophageal Reflux Disease. American Journal of Gastroenterology
- Risk factors for gastroesophageal reflux disease: a population-based study | BMC Gastroenterology | Full Text
